Top Benefits of Innovative Health Plans for Managed Care Providers

Managed care shifts healthcare delivery from a reactive system to a proactive one. By integrating networks of providers, prioritizing preventive care, and emphasizing performance-based incentives, managed care organizations (MCOs) deliver more efficient, cost-effective healthcare.
However, running high-performing medical management programs is no small feat. Payers must leverage data-driven strategies, align provider incentives, and optimize reimbursement structures while maintaining cost efficiency. Providers must also balance exceptional patient care with financial control while navigating an ever-shifting regulatory landscape.
With growing pressure to enhance operational performance and improve patient satisfaction, succeeding in a
value-based care model requires more than just experience—it calls for the right technology. Our latest blog explains why cutting-edge healthcare software is a must-have for
managed care providers and payers.
Advanced Solutions for Managed Care Organizations
Why Are Innovative Health Plans Important?
Innovative managed-care models improve the system by integrating technology, data-driven decision-making, value-based care models, and patient-centered approaches. These changes lead to better disease prevention, earlier diagnoses, and more personalized treatments.
Studies show that value-based health plans increase screening rates, vaccinations, and chronic disease management—all of which are key indicators of improved public health and wellness. Additionally, health insurers that implement modernized managed-care strategies tend to outperform competitors in assessments of healthcare quality and patient satisfaction, such as:
- Health Effectiveness Data and Information Set (HEDIS)
- Health Outcomes Survey (HOS)
- Consumer Assessment of Healthcare Providers and Systems (CAHPS)
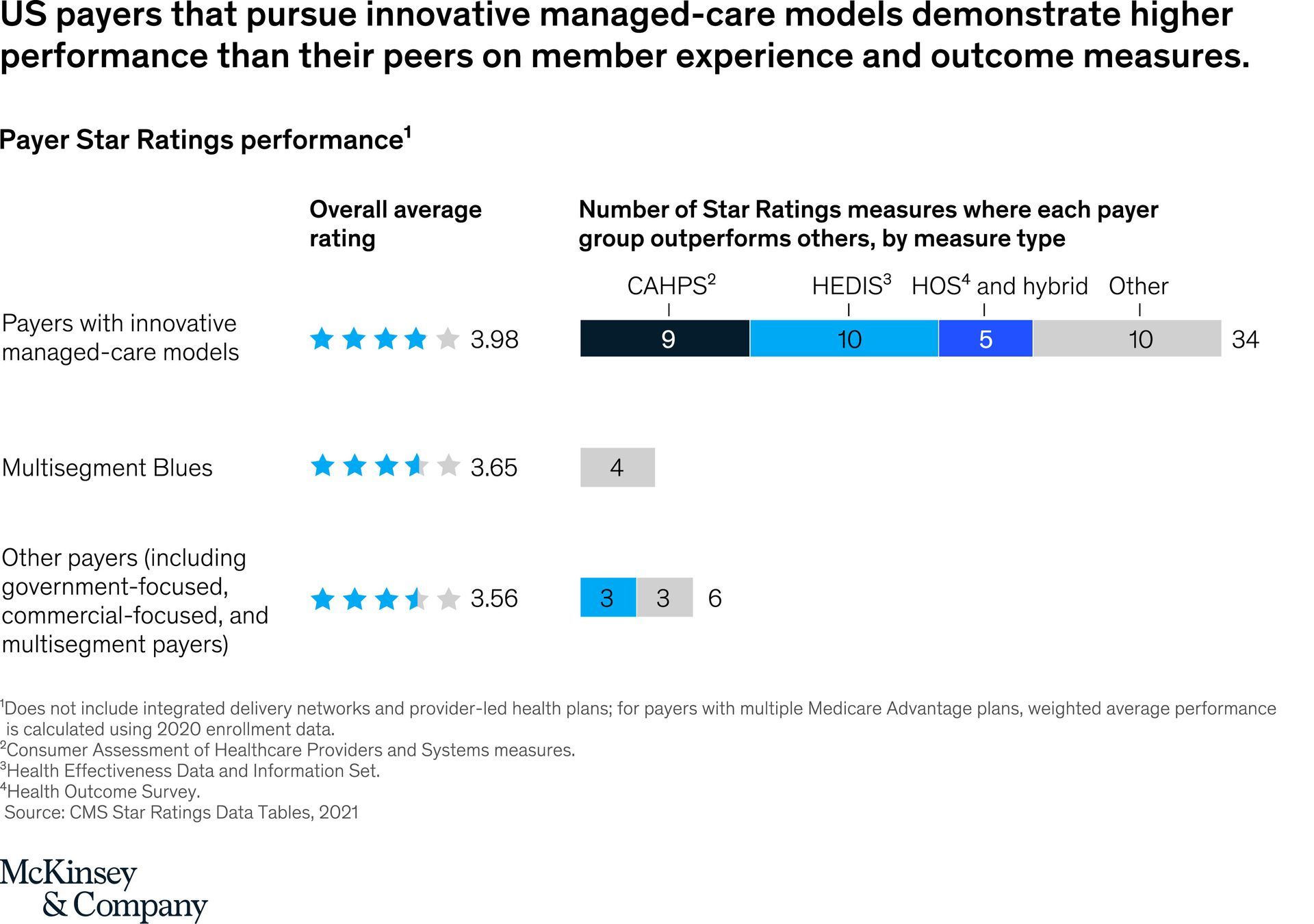
Source: McKinsey & Company
Benefits of Value-Based Managed Care Plans
Managed care is now the leading model for providing healthcare benefits, with over 74% of Medicaid beneficiaries enrolled in MCOs. States are using this framework to:
- Go beyond basic coverage.
- Enhance health equity.
- Close care gaps.
- Address key social determinants of health.
As a result, innovative health plans are driving measurable improvements such as:
1. Enhanced Patient Satisfaction
Patients want a healthcare experience that is personalized, efficient, and outcome-driven. Innovative managed care plans prioritize patient-centered models that:
- Expand access to care through telehealth, digital tools, and streamlined provider networks.
- Create personalized health plans that align with individual medical needs and preferences.
- Improve coordination among providers, ensuring seamless care transitions.
2. Higher Cost Efficiency
Rising healthcare costs are a concern for both patients and providers. MCOs with value-based care models are tackling inefficiencies by:
- Reducing unnecessary medical tests and procedures through data-driven decision-making.
- Using predictive analytics to identify high-risk patients and intervene early.
- Automating workflows to lower administrative costs.
Research by
McKinsey & Company found that investing in whole-person care could generate up to $185 billion in potential savings, proving that value-based managed care plans benefit everyone in the system.
3. Better Health Outcomes
Proactive, data-driven care management drives better health outcomes by:
- Using advanced analytics for population care management where the system can predict and prevent chronic conditions before they escalate.
- Integrating wellness programs that promote healthier behaviors, such as smoking cessation and nutrition counseling.
- Expanding access to preventive services, ensuring early detection and timely treatment.
- Enhancing provider networks, allowing patients more options and better accessibility to quality care.
4. Streamlined Operations
Technology-driven managed care plans reduce administrative complexity by:
- Automating claims processing and provider credentialing to reduce paperwork bottlenecks.
- Enhancing communication channels between patients, providers, and insurers through integrated digital platforms.
- Utilizing AI and machine learning to optimize resource allocation and workforce management.
5. Competitive Advantage
Health plans that embrace innovation set themselves apart from the competition by:
- Offering unique, member-driven services such as remote monitoring.
- Attracting and retaining members through value-added services like health outreach. programs, mobile clinics, and community-based wellness initiatives.
How MedVision Helps Managed Care Providers

Given the growing demand, MCOs cannot afford to use outdated processes. The healthcare industry is evolving, and the most successful organizations leverage integrated solutions.
MedVision’s QuickCap provides the tools to streamline operations, optimize care coordination, and ensure regulatory compliance—without adding administrative burden. Explore the features of our integrated, future-ready software system:
✔️ Advanced Patient Management System
QuickCap features an adaptable, user-friendly portal for both providers and members. This patient management system enhances accessibility and usability, ensuring that patient data, medical histories, and treatment plans are manageable and readily available.
✔️Efficient Authorization Management
Our platform enhances the efficiency of prior authorizations with a streamlined, automated system that reduces wait times and expedites approval processes. This ensures that patients receive necessary treatments without unnecessary delays.
✔️ Seamless Communication and Efficient Referral Systems
QuickCap integrates state-of-the-art communication tools to facilitate seamless referrals and enhance collaborative care between primary care physicians, specialists, and other care teams.
✔️ Integrated Preventative Care Strategies
Designed to support value-based care models, QuickCap incorporates proactive care strategies using embedded evidence-based guidelines to reduce disease incidence and improve long-term patient health outcomes.
✔️ Strategic Cost Management
Our platform delivers advanced capitation models for primary and specialty care that optimize financial performance and patient resource allocation.
✔️ Streamlined Claims Processing
QuickCap facilitates claims adjudication with an automated, rules-based processing system that significantly reduces manual effort, minimizes errors, and expedites reimbursements.
✔️ In-Depth Health Plan Auditing and Reporting Tools
Our software system features robust auditing tools and detailed reporting mechanisms that provide critical insights into health plan performance, compliance, and operational efficiencies.
✔️ Insightful Dashboards
QuickCap equips executives and department leaders with real-time, visually intuitive dashboards for better operations oversight and strategic decision-making.
✔️ Enhanced Data Security Protocols
The platform incorporates HIPAA-compliant EDI technologies to ensure the highest levels of data security and integrity during data exchanges.
Power Up Your Care Management Program with QuickCap!
For managed care providers ready to raise the bar, MedVision delivers solutions that optimize operations and enhance patient outcomes. More than just a technology provider, MedVision helps organizations redefine what’s possible—making value-based care more efficient, proactive, and patient-centered.
Unlock new levels of efficiency with QuickCap. Our advanced software for
healthcare administration programs gives you the edge to stay ahead in an evolving industry. Contact us for more information on our provider and
payer solutions.
Managed Care Needs More than Just a Good Plan—It Needs the Right Software!
Recently published articles
Keep in touch
Subscribe to get the latest update
Trending topics
Share your insights on social media
Upcoming events and company news












